Rare Disease Day 2022: Amy's Birdshot Uveitis Story
As part of Birdshot Uveitis Society of North America's efforts to commemorate Rare Disease Day 2022 on February 28th, this month BUSNA has shared the diagnosis story of four of our birdshot friends. As with other rare diseases, many people endure tremendous hardship before learning the name of their autoimmune disease.
Here is Amy's incredible story. Twenty years have passed since she started exhibiting Birdshot symptoms. Even though we think a proper diagnosis is likelier nowadays, we suspect that there are still some who are unaware of their birdshot uveitis.
I will never forget September 10, 2004. The night before I'd noticed that I couldn’t see anything out of my right eye, and it was very red. That morning I saw my ophthalmologist to see what was going on and he realized my central vision was completely gone. Then he immediately sent me to see a retinal specialist in West Monroe, LA.
That doctor did an eye exam and saw that the optic nerve was completely swollen shut in the right eye and was swollen in the left eye. I could not see any of the eye chart out of my right eye. I was told that he had never seen this before and was going to call a neurologist across town. The neurologist ran several kinds of tests and couldn’t figure out anything at all. He admitted me to the local hospital and started aggressive doses of Prednisone, where I also had a spinal tap and an MRI. He was convinced it was Multiple Sclerosis.
The spinal tap and MRI came back completely normal. We were getting nowhere, and I was so frustrated. After 5 days in the hospital, doing around the clock steroids, the inflammation had decreased some. I was sent home on Prednisone and was scheduled for a follow up the next week.
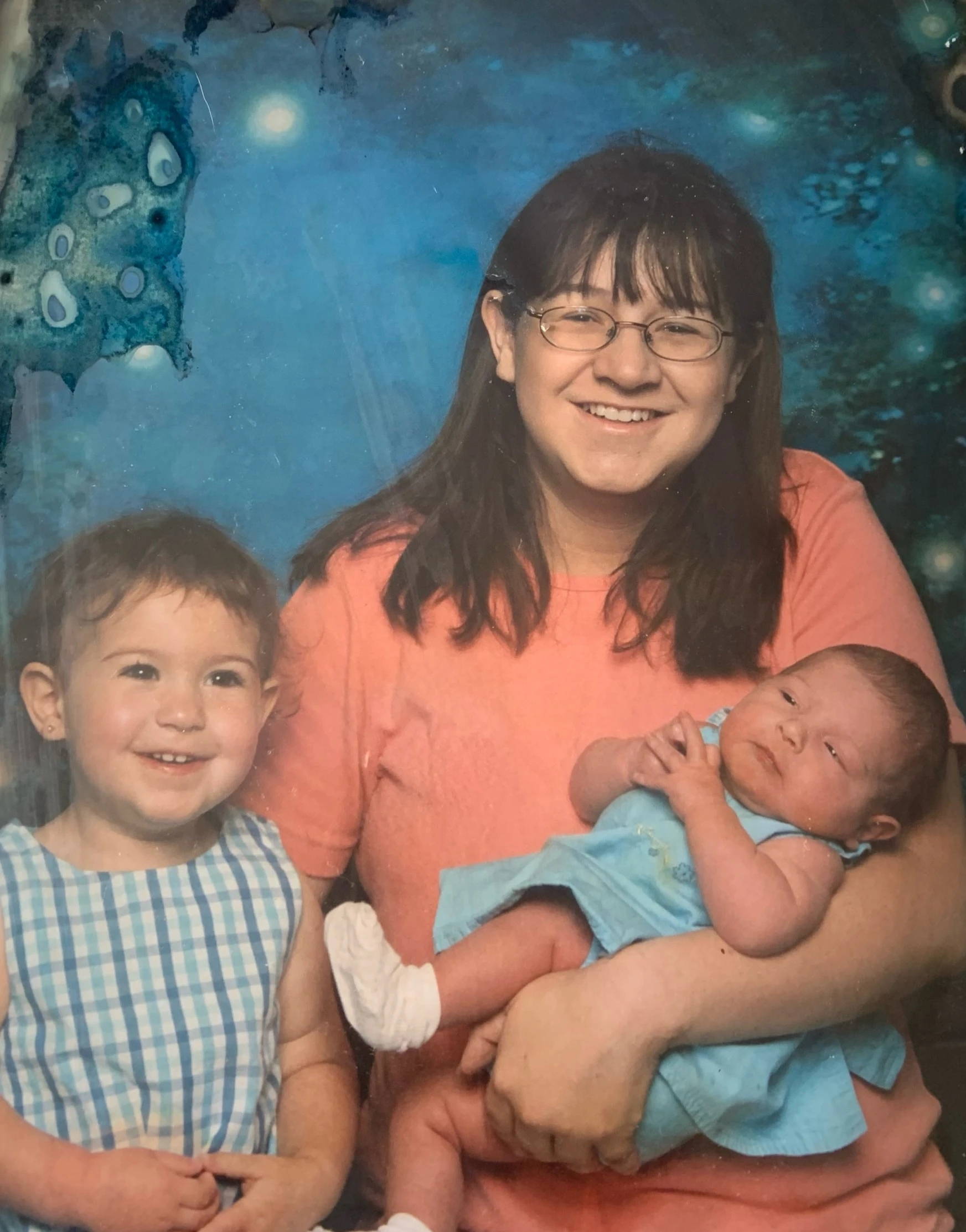
I was 21 years old with a two-year-old and a four-month-old at home. I couldn’t work and couldn't see well enough to mix bottles or even cook. The Prednisone was wearing me down already. I never slept, was gaining weight and just felt miserable. The frustration was insane. I waited impatiently for my follow up appointment.
When I arrived for the follow up with the neurologist, he looked into my eyes and saw the optic nerve completely swollen again in the right eye. The left eye was almost just as bad. He admitted me again and did high doses of steroids. He also wanted to try a chemotherapy drug that is used to treat breast cancer. Some studies had supported uses with optic nerve swelling. At that point we still had no idea what was going on. We continued the steroids, administered the chemotherapy drug and prayed it would work. Unfortunately, it did not.
At that point I was sent to see a retina specialist at an eye center in New Orleans, Louisiana. He took pictures with and without contrast and did an ERG. All the tests were showing significant damage to the optic nerve and massive amounts of macula edema. I was seeing 20/200 in the left eye and 20/400 in the right because of the swelling. I was told there was nothing else that could be done to stop the swelling or repair the damage. The steroids were just holding the inflammation at bay.
I gave up. I stopped working, could barely see to take care of my baby girls. I couldn’t cook or clean or do any of the things that I had taken for granted. I decided to see if there were any other doctors who could help.
I went back to Haik Humble Eye Care in November of 2004. I had no answers, had no idea what to do, and needed some explanation for what was happening. I was then referred to a vitreo retinal ophthalmologist in Shreveport, LA. I hoped he would be able to figure something out. The day of the visit I was in his office for 6 hours. He was the best in his field in our area. He checked my vision, and it was still holding at 20/200 in the left and 20/400 in the right. He did a visual field, an ERG and took pictures.
The macula edema was still bad. The doctor informed me that I had posterior uveitis. (Editor: This is a broad term for any number of diseases that cause inflammation of the choroid, the back part of the uvea. Posterior uveitis can be infectious or non-infectious. Birdshot uveitis is a non-infectious posterior uveitis, but treatment needs to be birdshot specific.) I was so excited because we finally had a diagnosis, or so I thought. He decided to add a steroid drop on top of the steroids by mouth and told me to come back in two weeks. I was hopeful for a few days, but it didn’t last long. I woke one morning and both eyes were hurting so bad. It hurt to open them. I couldn’t dare walk outside without sunglasses. I remember being so frustrated at that point. I was desperate to figure out what was going on.
The same ophthalmologist sent me to a rheumatologist to get his opinion. He was thinking maybe an immunosuppressant to go along with the steroids. The rheumatologist ran every blood test imaginable. He did x rays, bone scans, MRI and everything kept coming back normal. At that point he added Imuran to the Prednisone and told me he wanted me to see a retinal specialist at in Rochester, MN.
I just knew that we were going to get answers. We were going to one of the best medical facilities in the United States. It took a couple of months to get an appointment, so my retina specialist in Shreveport continued to treat me. The steroids, Imuran and Pred Forte drops were not controlling the symptoms. Every week the damage was getting worse.
He finally decided to try to steroid injections in the eye. That was one of the scariest moments in my life. It sounded horrible. I had no idea what to expect. Was it going to hurt?
How was I going to keep my eye open long enough? What if I moved and messed him up? My anxiety was out of control. Luckily, he talked me through it all. It was very simple. Within a week the swelling had improved. We were making progress, or so we thought...
The injections worked really well for about two weeks, until my eye pressure started climbing. Then the swelling came back. Thankfully at that time, February 2005, we were heading to Rochester for an appointment.
I was told I'd be seeing several doctors and I should plan to stay a week. I was so hopeful! We booked the flights, hotels, planned my daughters care and started praying about this appointment. I remember thinking this is it! No more wondering, we would get answers.
We arrived at the clinic and saw an ophthalmologist first. She was very up to date on eye diseases and felt optimistic that she would be able to figure it out. She looked in both eyes and decided to add a couple of doctors. She made appointments with a Retinal Specialist, Rheumatologist, Pulmonologist, Neurologist, and a Gastroenterologist. She was thinking it was Sarcoidosis.
I had an MRI, cat scan, upper and lower GI, lung scans, an insane amount blood drawn, ERG visual field, bone scan and pictures with and without contrast on both eyes. All my lab work came back normal except my Sed Rate and my bone scan. My sed rate was extremely high due to the inflammation in my eyes. The bone scan showed that I had osteoporosis and my right hip was showing signs of deterioration due to the steroids. I was 22 years old and felt like I was falling apart.
At that point they informed me that I had an autoimmune disease; they were just not sure which one. I had gone there with high hopes of having a diagnosis, but I did not get one. I was told the posterior uveitis was extremely active, and I had an autoimmune disease of some type. The doctors changed nothing at all on the treatment of my eyes. I was to stay on the Imuran, steroids and steroid injections if needed. They also added Actonal for the osteoporosis. Frustration, anxiety and depression was getting the best of me. We headed home with no more answers than we had come with.
From February of 2005 to August of 2008, I bounced between the rheumatologist and retinal
specialist. I had not been able to come off the steroids at all. I was overweight, my hair had fallen out and my vision was still poor - 20/80 in my right eye, 20/100 in my left.
Something triggered an awful flare in September of 2008. I called my rheumatologist, and he gave me steroid infusions and added Actemra and Methotrexate to my medicines. He also wanted me to see a new retinal specialist. My vision was back to 20/100 in right and 20/100 in left.
I saw the retinal specialist and, and he was going off my original readings from 2004. Needless to say, I was not impressed. He was excited that my vision was better, but I could not make him understand that I had gotten some of the vision back at one point, yet had lost it again. He told me that my rheumatologist and I were freaking out over nothing. The frustration was unbelievable.
I finished out the steroid infusions, took the Methotrexate and Actemra weekly and prayed it would work, but both of those meds stopped working in December. We could not find anything to keep the flares quiet. My rheumatologist was frustrated and didn’t really know what to do. He stopped the Methotrexate and the Actemra and decided to try Humira. I was willing to try anything.
He showed me how to inject and he wrote a new prescription for steroids. I got home that night, gave myself the injection, cooked supper and settled my daughters in for the night. By the time I slowed down and looked at my leg I realized it was swollen and the injection site had fever. I iced it and went to bed. When I woke up the next morning the swelling was worse, and I had streaks running down my leg. I called my doctor and he told me to go straight to the hospital. I had cellulitis in the injection site. Humira was no longer an option, and I was terrified. The thought of going completely blind was horrible. According to my doctor, we were running out of options.
He decided to try Cellcept as one last drug. He wasn’t sure it was going to be strong enough, but he wanted to give it a shot. The Prednisone was killing me slowly. I saw no end or hope in the future. I was resigning myself to going completely blind, not being able to take care of my daughters, and giving up teaching preschool. I was praying it wouldn’t happen but also praying for peace if it did. I just wanted a diagnosis and a plan, but I felt pretty sure that wasn’t going to happen.
Summer break was coming up for me and my daughters. I hoped the break would help. The Cellcept seemed to be working and I was able to taper down to 10mgs of steroid. I was finally getting some relief.
On my birthday in July of 2009, I woke up and could not see anything out of my right eye. Here we go again. I called Haik Humble and asked if there was any way I could be seen by a retinal specialist as soon as possible. I remember the receptionist saying we have a brand-new retina specialist. Dr. Jeffrey M. Gosslee, who just recently returned to Shreveport. She said he could squeeze me in that day. I wasn’t really expecting very much to happen. Nobody knew anything up till now so I’m sure he wouldn’t.
To be honest, I arrived at the appointment with a bad attitude. I wasn’t sure why I was even trying. I got in a room and the tech started the eye exam. My left eye is 20/100 and my right eye was 20/400. The swelling was bad in the front and the back of the eye. I sat through another visual field and countless pictures. I sat in the exam chair thinking about all the things I was going to miss seeing with my daughters as they grew up. I was slowly coming to terms with being blind.
I remember when Dr. Gosslee came in the room. By then I was 26 years old, and the doctor looked almost as young as I was. I remember thinking that this appointment would go nowhere.
Dr. Gosslee sat down and asked me to walk him through that everything that happened from the beginning up until then. We talked for an hour. He asked questions nobody had asked before and wrote down pages of notes. He then did the eye exam and explained everything he was seeing.
The damage was extensive because we had just been treating the symptoms. He told me we would probably never be able to correct everything. He also told me he had an idea of what this could possibly be but didn’t want to go any further until we ran a blood test.
He got on the phone with my rheumatologist, who immediately agreed to do the blook work. I then drove across town and had the labs drawn. I was told the results would be forwarded to Dr. Gosslee within two weeks. That was the longest two weeks of my life. I was hopeful and so ready to find out what was going on.
On the day of my appointment, I drove to his office, praying the whole way there, begging God to please let me get answers. As soon as Dr. Gosslee walked in the room he told me he had a diagnosis. I had waited almost 6 years to hear those words. He explained to me that I was positive for the HLA-A29 gene. He went on to explain that I had Birdshot Chorioretinopathy. Of course, I had no clue what that was.
He began to explain that the edema, the floaters, the flashes of light and the extreme vision loss was all caused by this disease. He explained to me that he did his internship under a Retina Specialist in Dallas Texas and had seen a few cases of this. He contacted this doctor and explained my case to him and asked if he would see me. It took us a few months to get an appointment but was so excited because we finally had a diagnosis.
I met Dr. Robert C. Wang at Texas Retina Associates in March of 2010. I had done a huge amount of research and had questions written down to ask him. He answered all of my questions and immediately started treating me. He started out with steroid pellets in both eyes that were supposed to last for three months. We decided he would administer the pellets and Dr. Gosslee would follow me closely since Dallas was a 5-hour drive. Unfortunately, the pellets only lasted a month. Dr. Gosslee called Dr. Wang to let him know that the pellets were no longer keeping the inflammation quiet. At that point Dr. Wang decided that Retisert implants would be our next option.
May 10,2010 I had my first Retisert implant surgery on my right eye. That was a nerve-wracking event for me. Dr. Wang walked me through procedure and informed of how things would work. The surgery went smoothly and the next morning everything was stable. I was told to return to the office in two weeks to see how my right eye was doing and discuss the surgery for my left eye.
In July of 2010 I had the Retisert implant put into my left eye. Both surgeries were a success. For the first time, I was in remission and my vision had returned. At my 6 month follow up I was told I could start tapering off the steroid by mouth. My vision had returned to 20/60 in right eye and 20/80 in left eye. I was so excited.
In March of 2011 my vision started deteriorating again. I immediately started panicking, because Dr. Wang said the implants should last 3-5 years. I made an appointment with Dr. Gosslee, knowing I was back in a flare. Once Dr. Gosslee did his exam he told me cataracts had formed due to all of the steroid shots and the steroid implants. He said that was an easy fix and scheduled cataract surgery. I had cataracts removed in both eyes in July of 2011.
After that my vision stayed stable until 2014, when I noticed a decrease in my vision. The floaters and flashes of light were increasing, and I could no longer drive safely. I called Dr.
Gosslee and Dr. Wang to let them know. Dr. Wang informed me to come back over to Dallas to see if the implants were empty. Once there, he told me that my implants, in fact, were empty and it was time for two more surgeries. In July of 2014 I had my fifth and sixth eye surgery. It was so worth it. I was back in remission!
A routine check-up in January 2015 revealed elevated pressure in both eyes. Eye drops helped control the pressure until August of that year, when Dr. Gosslee discovered it to be 58 in the left eye and 47 in the right. He and Dr. Wang sent me to a glaucoma specialist, Dr. Godfrey, the next morning in Dallas. Eye pressure was 62 and 57. He immediately scheduled glaucoma surgery to make the vents in my left eye to drain the fluid. That was by far the toughest surgery I had had, and although the pressure immediately dropped, I couldn't see anything.
It was frustrating not being able to work, drive, or do any of my daily things but I sat in the recliner and rested. We tried to wait to do the surgery on the right eye until after I got the vision back in my left eye, but we couldn’t wait any longer. The pressure was steadily climbing. Dr. Godfrey decided to place a shunt in the right eye instead of making the vents. The shunt surgery was less invasive, and I would still be able to see out of that eye while the left one healed.
My eighth surgery was to replace the shunt. When I came out of that surgery my right eye was patched and couldn’t see out of the left eye because the blood was still pooled in my line of vision. That was a terror I will never forget. I was scared to death and couldn’t see. I was completely dependent on the nurses and my mom. My pressure had gone down, but it wasn’t where Dr. Godfrey wanted it to be. I was told to go home rest and come back in two weeks.
At my post op appointment, my left eye was doing great, but pressure in my right eye was still 36. He had to go in and make the vents for the fluid to drain out. The surgery was a success, my pressure was down to 10 the next morning. I could finally take a breath and not worry as much. I stayed in remission for almost 2 years. I was so thankful for Jeffrey M. Gosslee, M.D. and Robert C. Wang, M.D. They gave me my vision back, which gave me my life back.
The Retisert implants have also given me my vision back. In 2017 I had to have the implants replaced again. Dr. Wang offered to do both eyes at the same time since I live so far from his office. The return trips and follow up appointments are a lot to deal with when I must drive 5 hours to his office. It is tough coming out of surgery and having both eyes patched but I have learned to adapt to it. In 2020 I had my fourth set of implants put in and I am still in remission. I do take Humira once a week and I must always keep rewetting drops with me, but I have come so far with this disease.
Every morning I wake up and immediately thank God for being able to see another day. This disease has taught me how to fight my battles and to always have compassion for others. We never know the daily battles that a person faces. I do not take for granted all the things that I am able to do and achieve while battling this disease. I have an amazing support system between family, friends and all our birdies.
Special thanks to Amy for helping us commemorate Rare Disease Day 2022. We're happy that her Birdshot is stable and wish her well as she continues on her journey!
The words, strategies, opinions, and treatment paths described here are that of one birdshot patient. BUSNA is not a medical organization and provides no medical advice. All birdshot patients are urged to follow the advice of their eye disease specialist who can monitor and help manage disease progression.
BUSNA encourages all those with birdshot uveitis to read the Birdshot Survival Guide for a broad view of the disease and its common practices.